Intracranial Monitoring
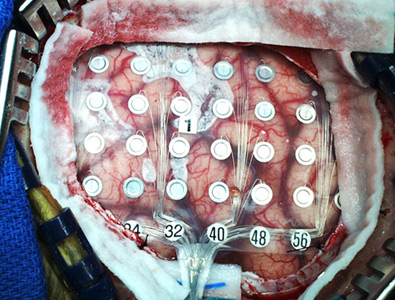
Intracranial monitoring refers to video-EEG monitoring where the EEG electrodes are placed inside the skull by a specially trained epilepsy neurosurgeon. The electrode placement is performed in the operating room with the patient asleep under general anesthesia. Typically, a series of electrodes are placed over the region or regions where seizures are thought to originate. After recovery from the surgery, the patient undergoes video-EEG monitoring in the epilepsy monitoring unit or the intensive care unit.
Intracranial monitoring is done on patients who are being evaluated for epilepsy surgery, when less invasive studies have not pinpointed the part of the brain where seizures start. Your doctor may recommend that you have intracranial monitoring if your seizures are severe, are not controlled with medications, and are probably coming from only one place in your brain. It is usually the last step before the actual removal of abnormal brain tissue. Intracranial monitoring serves two purposes. First, it allows the epilepsy team to be absolutely sure where seizures are starting so that the entire seizure "focus" is removed. Second, it allows the team to make sure that any important brain areas near the seizure focus will not be removed.
Prior to monitoring, your epilepsy physician will discuss your specific situation with the SUNY Downstate epilepsy team, including the epilepsy neurosurgeon, Dr. Ashesh Mehta. If the team agrees that the potential benefits of intracranial monitoring outweigh the risks, you will meet with the neurosurgeon who will answer your questions about the surgery. If you agree to go ahead with the procedure, it will be scheduled at a time convenient for your schedule. When you schedule the surgery it is important to remember that
What to Expect
After the surgeon places the electrodes, you will be taken to the intensive care unit or the Epilepsy Monitoring Unit for several days (rarely up to two weeks) of video- EEG monitoring. During this time your epilepsy medications may be reduced in order to provoke your typical seizures. The epilepsy team closely monitors these recordings until they understand where in your brain your seizures start.
If the area where the seizures start is close to critical brain regions, such as those that control language or movement, then additional testing is done to "map" exactly where those regions are so that the surgeon can avoid damaging them. The "brain mapping" procedure uses the electrodes lying on the surface of the brain to stimulate specific brain regions and see how this affects your ability to speak, move or feel. This testing is called cortical stimulation mapping.
After the epilepsy physicians review the seizure recordings and the stimulation mapping, they will discuss with you whether you are a good candidate for removing brain tissue to stop your seizures. They will give their impression, specific to you, about the likelihood of seizure freedom, and possible side-effects or disability that might occur.