Pancreatic Cancer
Pancreatic cancer is the fourth most common cause of cancer death in the U.S., according to the American Society of Clinical Oncology. Like other cancers the cause is a cell that starts making copies of it’s genetic material without any limitation or control. The risk of developing pancreatic cancer increases with age with most patient being diagnosed after the age of 65 and more commonly in males than in females. Tobacco smoking is one of the biggest risk factors for pancreatic cancer. Survival rates are impacted by tumor size and whether the cancer has spread to other organs.
 It is very difficult to catch this cancer early because initially it does not cause
any signs or symptoms, and there are no recommendations to screen for this cancer
these days. Therefore, pancreatic cancer is typically diagnosed at later stages, making
long-term prognosis and survival rates much lower than other cancers.
It is very difficult to catch this cancer early because initially it does not cause
any signs or symptoms, and there are no recommendations to screen for this cancer
these days. Therefore, pancreatic cancer is typically diagnosed at later stages, making
long-term prognosis and survival rates much lower than other cancers.
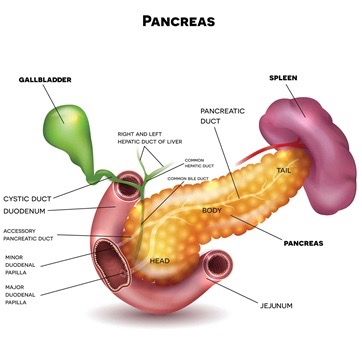
The location of the tumor within the pancreas can impact how soon signs and symptoms are first seen. In the head of the pancreas the tumor tends to grow to a size that blocks the duct that drains bile from the liver into the intestine and as a result your skin becomes yellow (jaundice), your eyes too (scleral icterus), your stool loses its color and you may experience itching of the skin (pruritus). If the tumor originates in the body or tail of the pancreas it usually takes longer to start causing symptoms such as pain, and therefore may be discovered later in the disease process and be associated with worse outcomes.
If your tumor has not spread to other organs and it can be safely removed surgically, which occurs in about one out of five patients presenting with pancreatic cancer, your overall chance of surviving is higher than patients who cannot have their tumors removed surgically.
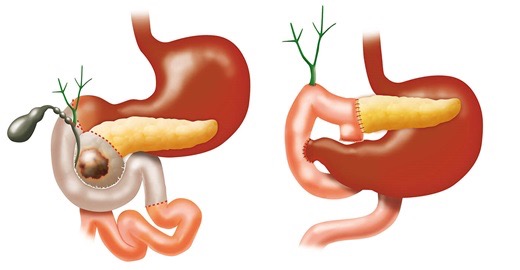
The mainstay of therapy for early pancreatic cancer that has not spread to other organs and does not significantly involve the major blood vessels is surgical resection, often in combination with chemotherapy either before or after the surgery. The type of operation depends on the location of the tumor. Tumors of the head of the pancreas are treated with the Whipple procedure (hyperlink) and tumors of the body and tail of the pancreas with a distal pancreatectomy which can be performed by minimally invasive techniques (laparoscopy). Laparoscopic procedures are performed using small incisions in the abdomen through which telescope-guided instruments are placed.
Whipple procedure: The Whipple procedure (also called a pancreaticoduodenectomy) is the primary surgical treatment for pancreatic cancer that occurs within the head of the pancreas. During this procedure, surgeons remove the head of the pancreas, most of the duodenum (a part of the small intestine), a portion of the bile duct, the gallbladder and associated lymph nodes. The need to remove all these organs comes from the joint blood supply and lymph drainage. On average, the surgery takes six hours to complete. Most patients stay in the hospital for one week following the Whipple procedure.
Nutritional consideration for the patient with pancreatic cancer
Common nutrition problems that may arise with pancreatic cancer before or after surgery include:
- Unexplained weight loss
- Malabsorption due to pancreatic insufficiency
- Development of diabetes
- Loss of appetite
- Taste changes/ metallic taste
- Nausea
Nutritional intervention for pancreatic cancer includes a) small, frequent meals, b) high protein meals, c) oral nutrition supplement use, d) whole grains and healthy fats consumption, and e) physical activity as able. Food items that are high in sugar and not easy to digest are not recommended. In patients who have lost more than 10% of their baseline weight, alternative means of nutrition should be considered.
Nutrition intervention summarized:
- Treatment of weight loss: small, frequent, nutrient-rich meals with early satiety and anorexia
- Treatment of fat malabsorption: patient may likely need pancreatic enzymes with suspected or diagnosed malabsorption and weight loss
- Blood glucose control: promote glycemic control with constant carbohydrate intake
- For prolonged poor appetite: consider appetite stimulants such as megestrol acetate or dronabinol
- Incorporate physical activity such as walking to help preserve lean body mass
Patients may consider oral nutritional supplements and nutrient-dense nourishments to maximize calorie and protein intake.