Become a Certified Coding Specialist (CCS®) or Certified Professional Coder (CPC®)
SUNY Downstate Health Sciences University, School of Health Professions Medical Billing and Coding program is a certificate program designed to assist individuals entering the field of medical billing and coding, or preparing for certification. The American Academy of Professional Coders (AAPC) 2015 data showed that the average wage for a Certified Professional Coder (CPC®) was approximately $50,000. The Billing and Coding program is a part-time evening and weekend program.
Register for Virtual Information Session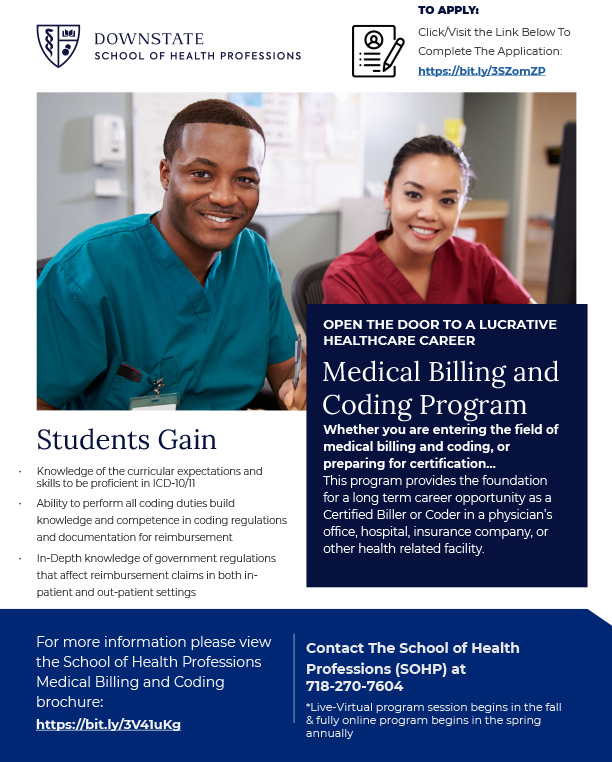
Medical Billing and Coding Flyer
Medical Billing and Coding Online Application